Procedures
Spine surgery has a reputation for being the “last stop.” That may have been true once upon a time, but not anymore.

Advanced Technolgy
Technology today is light years ahead of where it once was. Procedures that once took many hours to perform with days spent in the hospital and months spent in recovery, can now be done in one to three hours with a simple overnight stay in the hospital, or even home the same day.

Minimally Invasive
In fact, patients undergoing spine surgery with Dr. Reddy will be happy to know that nearly all procedures he performs are minimally invasive – meaning smaller incisions, less muscle and tissue disruption, faster recovery, and better outcomes. Some he is even able to perform robotically.

Optimal Outcomes
Although it depends on the patient’s individual condition and surgical procedure, most people who receive minimally invasive spinal surgery enjoy a rapid and more complete recovery following surgery.
Specialized Procedures

Adult Scoliosis
Normally, the spine has two gentle front-to-back curves that work in harmony to keep the body’s center of gravity aligned over the hips and pelvis. However, if one of those curves becomes too pronounced, as in the case of adult scoliosis, the spine will be out of balance back-to-front.
This condition – called sagittal imbalance – can cause symptoms that include pain and stiffness in the lower back; numbness, cramping, or shooting pain in the legs; fatigue due to unusual strain on muscles, back, and legs; abnormal gait; uneven shoulders and hip; difference in leg lengths; more prominent rib or shoulder blade when you bend. In severe cases, it may also cause breathlessness.
To more precisely and predictably correct the deformity in his patients, Dr. Reddy takes a very mathematical approach.
“We’ve learned a lot about adult scoliosis in contemporary spine research, and what we have realized is that there is a lot of variability in the care patients are receiving,” Dr. Reddy explained. “By looking at the spine as a complex physics problem, I am able to clarify how much surgery a patient needs to achieve the desired outcome.”
CERVICAL DISC
REPLACEMENT
Cervical disc replacement is a minimally invasive spine surgery Dr. Reddy performs to replace a damaged disc in the neck with an artificial disc. The artificial disc is designed to replicate the natural motion of the cervical spine to preserve range of motion in that area of the neck. At the same time, the artificial disc restores the height between two cervical vertebrae and relieves the pressure on the spinal nerves.
Dr. Reddy typically performs this surgery for patients who have cervical disc herniation or cervical degenerative disc disease that causes chronic neck and/or arm pain that hasn’t been relieved by non-surgical treatments.
The procedure is designed to relieve the pressure on your spinal cord or nerves that are causing the pain, numbness, and weakness that can radiate to your shoulder, arm, and hand.
Dr. Reddy performs cervical disc replacement through a small incision on the front of your neck. After he removes the damaged disc, he will smooth away any bone spurs and then place and anchor the artificial disc in the empty space that is left. After checking the range of motion of the neck and confirming the proper fit of the artificial disc, Dr. Reddy then closes the incision and covers it with a dressing.


Complex Cervical
Spine Surgery
Any spine surgery requires surgical skill, but complex cervical spine surgery is one of the most difficult to perform and requires a surgeon to be at the highest skill level.
Complex cervical spine surgeries are those that involve two or more vertebrae in the neck and require two or more hours of surgery.
In addition, some procedures are simply considered more complex than others. These include:
- Anterior Cervical Discectomy with Fusion (ACDF)
- Anterior Cervical Discectomy
- Cervical Corpectomy
- Cervical Foraminotomy
- Cervical Laminectomy
- Cervical Laminoplasty
- Anterior Cervical Corpectomy and Fusion
Dr. Reddy is highly trained in complex cervical spine surgery and uses advanced techniques to ensure that his patients receive maximum outcomes.
Lumbar Decompression
Lumbar decompression is a general term used to refer to various surgical procedures that are performed to alleviate pain caused when nerves become trapped (called neural impingement) in the spine’s lumbar (lower back) area.
During lumbar decompression surgery, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed to give the nerve root more space and provide a better healing environment.
Some of the procedures Dr. Reddy performs to decompress nerves in the lumbar area are:
Minimally Invasive Discectomy
This minimally invasive procedure is performed to relieve pressure on the spinal nerve column caused by a herniated lumbar (lower back) disc. During the procedure, Dr. Reddy will make a small incision and remove the disc material that is placing pressure on the nerves. The goal of the procedure is to decrease pain and allow you to regain normal movement and function.
Minimally Invasive Laminectomy
With a lumbar laminectomy. your spinal canal in the lumbar area (lower back) is enlarged through the removal of the lamina – the back part of a vertebra covering your spinal canal. Dr. Reddy performs a lumbar laminectomy to relieve pressure on the spinal cord or nerves caused by bone spurs within the spinal canal.
Resection of Facet Cysts
Facet cysts – also known as synovial cysts – are fluid-filled sacs located in the joints of the spine, most commonly in the lumbar section. They typically develop as a result of age-related degeneration of the spine.
Symptoms vary depending on the size and location of the cyst but generally include back or leg pain that worsens when standing and walking as well as numbness, tingling, or weakness in one or both legs. Facet cysts may also cause sciatica, which would likely present as pain in one or both legs which typically radiates to the foot.
Dr. Reddy’s typical treatment plan includes removing the cyst and decompressing the spinal cord and nerves. After removing the cyst, he may also need to fuse the joint to prevent the cyst from reoccurring and prevent any further instability of the affected joint.
Spinal Stenosis
Spinal stenosis of the back is usually a slow process that occurs over years results in thickening of the ligaments, formation of bone spurs, and deterioration of the disc material. As a result, the spinal canal narrows and pinches the nerves. Bone spurs may also press on the spinal cord.
Surgery may be necessary if lumbar stenosis limits normal activity, causes leg weakness and/or numbness, makes standing or walking difficult, or affects your ability to control of bowel and bladder functions. If Dr. Reddy feels surgery is your best option, he will take the least invasive approach he can that will give you the optimal outcome and will fully discuss his recommended procedure with you.

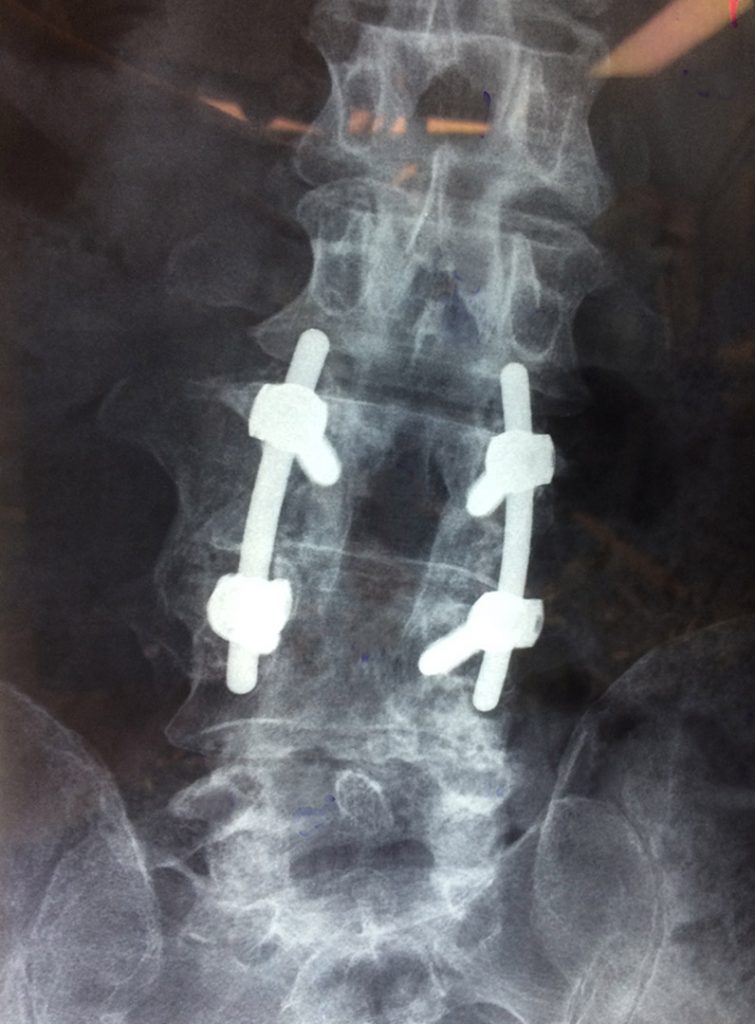
Lumbar Fusion
Lumbar fusion surgery is designed to permanently connect two or more vertebrae in your lower back to stop painful motion between vertebrae by “fusing” them together. Most commonly, this type of surgery is performed to alleviate the pain and disability caused by conditions such as degenerative disc disease or spondylolisthesis, although it can also be used to strengthen a weak or unstable lumbar spine, fractures, scoliosis, or deformity.
There are many different approaches to lumbar fusion and all involve techniques designed to mimic the normal healing process of broken bones. During your lumbar spinal fusion, Dr. Reddy places a bone graft or bone-like material within the space between two lumbar vertebrae. Metal plates, screws, and rods may be used to hold the vertebrae together so they can heal as one solid unit.
Some of the lumbar fusion procedures Dr. Reddy performs include:
Anterior Lumbar Interbody Fusion (ALIF)
The ALIF is one of the most frequently used spinal fusion techniques and is performed through the front of the body (anterior approach). Interbody fusion refers to the removal of an intervertebral disc, which is replaced with a spacer during the fusion process. A major advantage of anterior entry is that a larger implant can be incorporated into the procedure.
Anterior to Psoas Lateral Interbody Fusion
An Anterior to Psoas approach allows insertion of a lateral interbody cage at right angles to the spine at any lumbar level. These lateral interbody cages restore and maintain disc height while adding stability prior to supplemental fixation.
Fracture Fixation
The basic goal of fracture fixation is to stabilize the fractured bone, to enable fast healing of the injured bone, and to return early mobility and full function of the injured extremity.
Midline Cortical Screw Fixat
Allows a midline surgical approach for minimal tissue and muscle retraction, sparing the multifidus and other surrounding anatomy.
Minimally Invasive Lumbar Fusion
With minimally invasive lumbar fusion surgery, Dr. Reddy uses a smaller incision than traditional surgery to correct issues with the lower back. It also doesn’t cut away the muscles of your spine. Because of this, it typically leads to faster recovery times than traditional surgery.
Transforaminal Lumbar Interbody Fusion (TLIF)
Dr. Reddy performs the TLIF procedure through an incision made in the patient’s back. This approach can be advantageous since it avoids interfering with the many organs and major blood vessels that are present in the abdominal region. Interbody fusion involves removing an intervertebral disc, replacing it with a spacer and fusing the two vertebrae on either side of the spacer together. The goal of the TLIF procedure is to provide relief from the pain associated with a number of lower back problems such as spondylolisthesis and disc degeneration, which have not responded to non-surgical treatments.
Tumor Resection
Surgery is a common approach to cancer treatment, and surgical resection of a tumor can be performed for many types of cancer. The goal of surgery is to remove the entire tumor or as much of the tumor as possible.
Revision spine
Surgery
It’s an unfortunate truth that even with meticulously executed spine surgeries, complications can sometimes happen. Some patients won’t heal well, others don’t receive the outcomes they hope for.
When this happens, patients often assume there is nothing else that can be done to help them – but this isn’t necessarily true. While revision spine surgery is more technically demanding, Dr. Reddy is one of very few surgeons who are skilled enough to specialize in it.
To this end, Dr. Reddy has created a protocol for revision procedures that includes:
- Careful diagnosing of the patient’s individual issues
- Determining why surgery did not provide the desired outcome
- When indicated, performing restorative surgery to undo or redo a portion of the initial operation to provide pain relief
Some examples of the revision spine surgeries Dr. Scheid performs include minimally invasive nerve decompression, exploration of spinal fusions, and surgery for adjacent level diseases.
Even patients who have been told that nothing more can be done to relieve their pain may be candidates for revision spine surgery with Dr. Reddy.

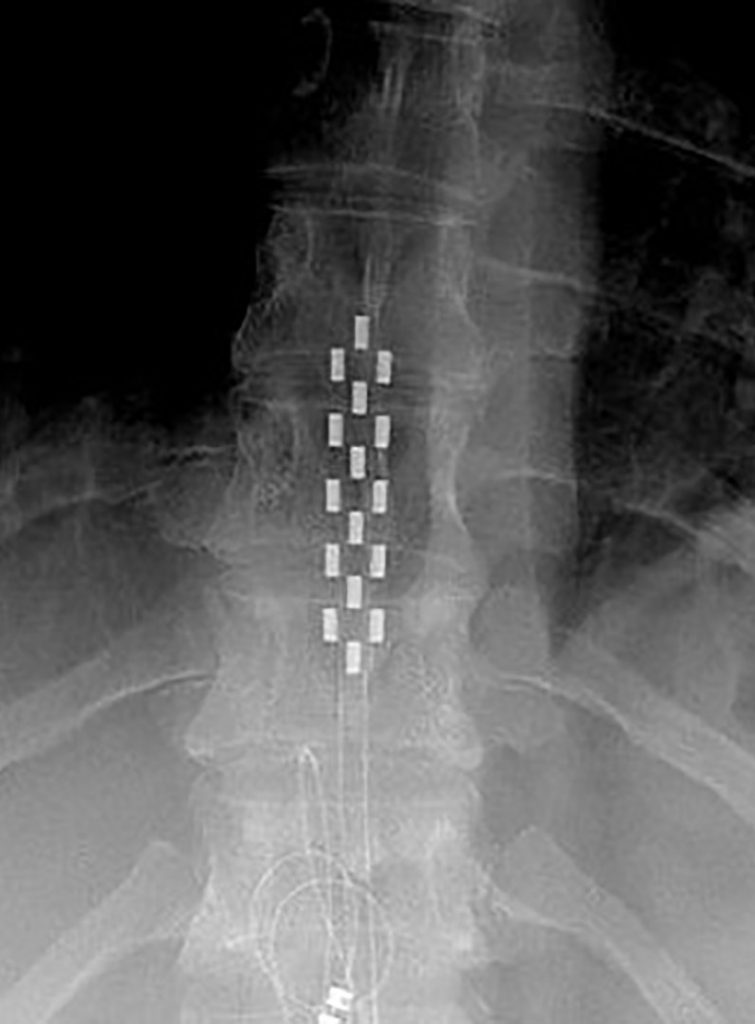
Spinal Cord Stimulation
People who suffer from chronic pain that isn’t sufficiently relieved by conservative, nonsurgical treatments may finally find relief through Spinal Cord Stimulation (SCS). Dr. Reddy uses SCS to treat and manage different types of chronic pain, including:
- Nerve-related back pain
- Spinal cord injuries
- Post-surgical pain
- Arachnoiditis (painful inflammation of the arachnoid, a thin membrane that covers the brain and spinal cord)
SCS works by disrupting the pain signals that travel between the spinal cord and the brain.
During the SCS treatment procedure, Dr. Reddy surgically implants a small device similar to a pacemaker under the skin, in close proximity to the spine. The device – called a neurostimulator – then sends a mild electric current to the spinal cord. Thin wires – called leads – carry current from a pulse generator to the nerve fibers of the spinal cord. When activated, the SCS stimulates the nerves in the area where pain is felt. Pain is reduced because the electrical pulses modify and mask the pain signals before they reach your brain.
SI Joint
Fusion
SI joint fusion is a minimally invasive surgical option Dr. Reddy performs to provide immediate sacroiliac (SI) joint stabilization and allow long-term fusion.
What is the SI joint?
Your sacroiliac joints connect your hip bones to either side of your sacrum (tail bone). It is an essential component for shock absorption to prevent impact forces from reaching the spine. When problems in that area occur, it can cause significant low back pain and sometimes the buttocks and legs. Degenerative joint issues, traumatic injury, or inflammatory joint disease are the most common reasons SI joint fusion may be recommended.
How is SI joint fusion performed?
After making small incisions on your hip, Dr. Reddy uses X-ray scans to view where instrumentation needs to go. He will then drill holes in the sacrum and ilium where he places implants to make the joint more stable. Dr. Reddy may also place a bone graft to the ilium to encourage bone growth across the joint. Fusion occurs during the healing process following the surgery.


